Retinal Detachment, Retinal Holes and Tears
What is a retinal detachment?
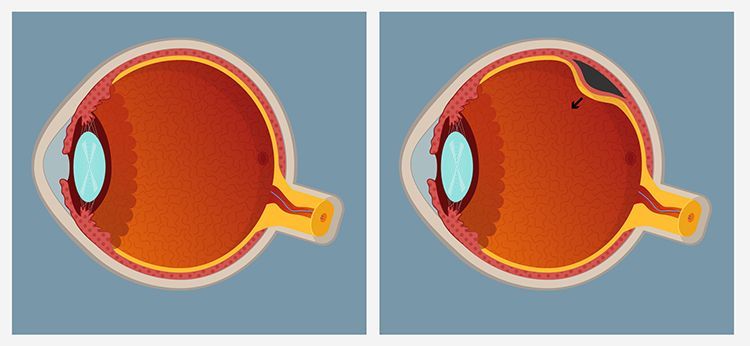
The retina is the light-sensitive layer of tissue that lines the inside of the eye and sends visual messages through the optic nerve to the brain. When the retina detaches, it is lifted or pulled from its normal position. If not promptly treated, retinal detachment can cause permanent vision loss.
What are retinal holes and tears?
In some eyes there may be small areas of the retina that are torn, or holes may develop. These areas, called retinal breaks, can lead to retinal detachment. Retinal breaks are often caused by traction from the vitreous, the gel that fills the back of the eye. Traction can occur as the vitreous pulls away from the retina, which occurs with age, trauma, surgery, inflammation, and near sightedness.
Who is at risk for retinal detachment?
A retinal detachment can occur at any age, but it is more common in people over age 40. It affects men more than women and Caucasians more than African Americans.
A retinal detachment is also more likely to occur in people who:
- Are nearsighted
- Have had a retinal detachment in the other eye
- Have a family history of retinal detachment
- Have had cataract surgery
- Have other eye diseases or disorders, such as retinoschisis, uveitis, degenerative myopia, or lattice degeneration
- Have had an eye injury
What are the symptoms of retinal breaks and retinal detachments?
Symptoms include a sudden or gradual increase in either the number of floaters, which are little “cobwebs” or specks that float about in your field of vision, and/or light flashes in the eye. Floaters and flashes may indicate that your retina has developed a break. Another symptom is the appearance of a curtain over the field of vision, which can indicate that the retina has detached. Sometimes, there are no preceding symptoms.
Retinal detachments and retinal breaks are urgent conditions. Anyone experiencing the symptoms of a retinal detachment or retinal break should see an eye care professional urgently.
Can retinal detachment be prevented?
Sometimes, retinal tears and holes (breaks in the retina which cause retinal detachments) can be treated before the retina detaches. During laser surgery, tiny burns are created around breaks in the retina to cause an adhesion to form, “welding” the retina around the break and keeping the retina in place. Occasionally, freezing is used to create an adhesion instead of laser. These procedures usually prevent the retina from detaching.
How is retinal detachment treated?
Retinal detachments can sometimes be treated by in-office surgery. Sometimes, it is appropriate to surround the area of detached retina with laser burns, which “weld” the retina in place. This procedure can be appropriate if the area of detached retina is small and located away from the area of central vision. Sometimes, gas can be injected into the eye, which can be used to seal the break or breaks in the retina and push the retina back in place. Laser or freezing can be used to create a “weld” around the break that caused the detachment. Special positioning of the head may be required if gas is injected into the eye.
Retinal detachments may also be treated with surgery in the operating room. In some cases a scleral buckle, a small synthetic band, is attached to the outside of the eye to gently push the wall of the eye against the detached retina. A vitrectomy may also be performed. During a vitrectomy, the doctor makes tiny incisions in the eye. Next, small instruments are placed into the eye to remove the gel that fills the back of the eye, called vitreous. Gas is often injected into the eye to replace the vitreous and reattach the retina; the gas pushes the retina back against the wall of the eye. During the healing process, the eye makes fluid that gradually replaces the gas and fills the eye. With all of these procedures, either laser or freezing is used to “weld” the retina back in place.
With modern therapy, over 90 percent of those with a retinal detachment can be successfully treated, although sometimes a second treatment is needed. However, the visual outcome is not always predictable. The final visual result may not be known for up to several months following surgery. Even under the best of circumstances, and even after multiple attempts at repair, treatment sometimes fails and vision may eventually be lost. Visual results are best if the retinal detachment is repaired before the macula (the center region of the retina responsible for fine, detailed vision) detaches. That is why it is important to contact an eye care professional urgently if you see a sudden or gradual increase in the number of floaters and/or light flashes, or a dark curtain over the field of vision. Visual results are often better still if retinal breaks are treated before they cause the retina to detach.